The Covid-19 oxygen crisis: How did we get here? Part 3. Pandemic preparedness
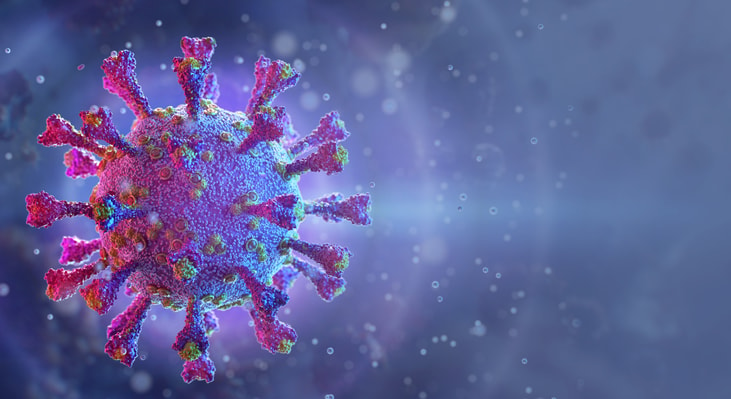
From the moment the SARS-CoV-2 virus first began to proliferate out of control in China and was subsequently recognised as a pandemic in official terms by the World Health Organization on 11th March 2020, it became one of the fastest-spreading and most significant pandemics in modern history.
It has been a once-in-a-century global pandemic that has so unexpectedly and irrevocably changed the world, in ways we could once have only imagined in big box office hits on the silver screen. But should we have left such imagination to great works of fiction?
We are familiar with influenza or the ‘flu’ as we so often affectionately seem to refer to it, and we are also reluctantly accustomed to flu pandemics of different variations. Indeed, a June 2013 WHO guidance document clearly states that, “Influenza pandemics are unpredictable but recurring events that can have consequences on human health and economic wellbeing worldwide. Advance planning and preparedness are critical to help mitigate the impact of a pandemic.” 30
... to continue reading you must be subscribed